Predictors Of Difficult Intubation: Study In Kashmiri Population
Arun Kr. Gupta , Mohamad Ommid , Showkat Nengroo , Imtiyaz Naqash and Anjali Mehta
Cite this article as: BJMP 2010;3(1):307
|
| ABSTRACT Airway assessment is the most important aspect of anaesthetic practice as a difficult intubation may be unanticipated. A prospective study was done to compare the efficacy of airway parameters to predict difficult intubation. Parameters studied were degree of head extension, thyromental distance, inter incisor gap, grading of prognathism, obesity and modified mallampati classification. 600 Patients with ASA I& ASA II grade were enrolled in the study. All patients were preoperatively assessed for airway parameters. Intra-operatively all patients were classified according to Cormack and Lehane laryngoscopic view. Clinical data of each test was collected, tabulated and analyzed to obtain the sensitivity, specificity, positive predictive value & negative predictive value. Results obtained showed an incidence of difficult intubation of 3.3 % of patients. Head and neck movements had the highest sensitivity (86.36%); high arched palate had the highest specificity (99.38%). Head and neck movements strongly correlated for patients with difficult intubation. KEYWORDS Intubation, Anaesthesia, Laryngoscopy |
The fundamental responsibility of an anesthesiologist is to
maintain adequate gas exchange through a patent airway. Failure to
maintain a patent airway for more than a few minutes results in brain
damage or death1. Anaesthesia in a patient with a difficult
airway can lead to both direct airway trauma and morbidity from hypoxia
and hypercarbia. Direct airway trauma occurs because the management of
the difficult airway often involves the application of more physical
force to the patient’s airway than is normally used. Much of the
morbidity specifically attributable to managing a difficult airway comes
from an interruption of gas exchange (hypoxia and hypercapnia), which
may then cause brain damage and cardiovascular activation or depression2.
Though endotracheal intubation is a routine procedure for all
anesthesiologists, occasions may arise when even an experienced
anesthesiologist might have great difficulty in the technique of
intubation for successful control of the airway. As difficult intubation
occurs infrequently and is not easy to define, research has been
directed at predicting difficult laryngoscopy, i.e. when is not possible
to visualize any portion of the vocal cords after multiple attempts at
conventional laryngoscopy. It is argued that if difficult laryngoscopy
has been predicted and intubation is essential, skilled assistance and
specialist equipment should be provided. Although the incidence of
difficult or failed tracheal intubation is comparatively low, unexpected
difficulties and poorly managed situations may result in a life
threatening condition or even death3.
Difficulty in intubation is usually associated with difficulty in
exposing the glottis by direct laryngoscopy. This involves a series of
manoeuvres, including extending the head, opening the mouth, displacing
and compressing the tongue into the submandibular space and lifting the
mandible forward. The ease or difficulty in performing each of these
manoeuvres can be assessed by one or more parameters4.
Extension of the head at the atlanto-occipital joint can be
assessed by simply looking at the movements of the head, measuring the
sternomental distance, or by using devices to measure the angle5.
Mouth opening can be assessed by measuring the distance between upper
and lower incisors with the mouth fully open. The ease of lifting the
mandible can be assessed by comparing the relative position of the lower
incisors in comparison with the upper incisors after forward protrusion
of the mandible6. The measurement of the mento-hyoid distance and thyromental distance provide a rough estimate of the submandibular space7.
The ability of the patient to move the lower incisor in front of the
upper incisor tells us about jaw movement. The classification provided
by Mallampati et al8 and later modified by Samsoon and Young9
helps to assess the size of tongue relative to the oropharynx.
Abnormalities in one or more of these parameters may help predict
difficulty in direct laryngoscopy1.
Initial studies attempted to compare individual parameters to predict difficult intubation with mixed results8,9. Later studies have attempted to create a scoring system3,10 or a complex mathematical model11,12.
This study is an attempt to verify which of these factors are
significantly associated with difficult exposure of glottis and to rank
them according to the strength of association.
read more..........
read more..........
Materials & methods
The study was conducted after obtaining institutional review board
approval. Six hundred ASA I & II adult patients, scheduled for
various elective procedures under general anesthesia, were included in
the study after obtaining informed consent. Patients with gross
abnormalities of the airway were excluded from the study. All patients
were assessed the evening before surgery by a single observer. The
details of airway assessment are given in Table I.
Table I: Method of assessment of various airway parameters (predictors)
Airway Parameter
|
Method of assessment
|
Modified Mallampati Scoring
|
Class I: Faucial pillars, soft palate and uvula visible.
Class II: Soft palate and base of uvula seen
Class III: Only soft palate visible.
Class IV: Soft palate not seen
Class I & II : Easy Intubation
Class III & IV: Difficult Intubation
|
Obesity
|
Obese BMI (≥ 25)
Non Obese BMI (< 25)
|
Inter Incisor Gap
|
Distance between the incisors with mouth fully open(cms)
|
Thyromental distance
|
Distance between the tip of thyroid cartilage and tip of chin, with fully extended(cms)
|
Degree of Head Extension
|
Grade I ≥ 90◦
Grade II = 80◦-90◦
Grade III < 80◦
|
Grading of Prognathism
|
Class A: - Lower incisor protruded anterior to the upper incisor.
Class B: - Lower incisor brought edge to edge with upper incisor but not anterior to them.
Class C: - Lower incisors could be brought edge to edge.
|
In addition the patients were examined for the following.
- High arched palate.
- Protruding maximally incisor (Buck teeth)
- Wide & short Neck
Direct laryngoscopy with Macintosh blade was performed by an anaesthetist who was blinded to preoperative assessment.
Glottic exposure was graded as per Cormack-Lehane classification13 (Fig 1).
Figure 1: Cormack-Lehane grading of glottic exposure on direct laryngoscopy
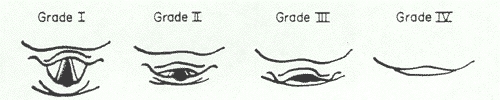
Grade 1: most of the glottis visible; Grade 2: only the
posterior extremity of the glottis and the epiglottis visible; Grade 3:
no part of the glottis visible, only the epiglottis seen; Grade 4: not
even the epiglottis seen. Grades 1 and 2 were considered as ‘easy’ and
grades 3 and 4 as ‘difficult’.
Results
Glottic exposure on direct laryngoscopy was difficult in 20 (3.3%) patients.
The frequency of patients in various categories of ‘predictor’ variables is given in Table-II
Table II: The frequency analysis of predictor parameters
Airway Parameter
|
Group
|
Frequency (%)
|
Modified Mallampati Scoring
|
Class 1&2
Class 3&4
|
96%
4%
|
Obesity
|
Obese BMI (≥ 25)
Non Obese BMI (< 25)
|
28.7%
71.3%
|
Inter Incisor Gap
|
Class I : >4cm
Class II: <4cm
|
93.5%
6.5%
|
Thyromental distance
|
Class I: ≥ 6cm.
Class II: ≤6cm.
|
94.6%
5.4%
|
Head & Neck Movements
|
Difficult {class II & III (90˚)}
Easy {class I(>90˚)}
|
16%
84%
|
Grading of Prognathism
|
Difficult (class III)
Easy (class I + II)
|
96.1%
3.9%
|
Wide and Short neck
|
Normal neck body ratio 1:13
Difficult (Ratio≥ 1:13)
|
86.9%
13.1%
|
High arched Palate
|
Yes
No
|
1.9%
98.1%
|
Protruding Incisors
|
Yes
No
|
4.2%
95.8%
|
The association between different variables and difficulty in
intubation was evaluated using the chi-square test for qualitative data
and the student’s test for quantitative data and p<0.05 was regarded
as significant. The clinical data of each test was used to obtain the
sensitivity, specificity and positive and negative predictive
values. Results are shown in Table III.
Table III: Comparative analysis of various physical factors and scoring systems
Physical factors and various Scoring Systems
|
Sensitivity ( % )
|
Specificity ( % )
|
PPV
( % )
|
NPV
( % )
|
Obesity
|
81.8
|
72.76
|
6.34
|
99.43
|
Inter incisor gap
|
18.8
|
94.14
|
6.6
|
98.1
|
Thyromental distance
|
72.7
|
96.5
|
32.0
|
99.4
|
Head and Neck movement
|
86.36
|
86.0
|
34.6
|
99.7
|
Prognathism
|
4.5
|
96.3
|
2.7
|
97.9
|
Wide and Short neck
|
45.5
|
87.9
|
7.8
|
98.6
|
High arched palate
|
40.1
|
99.38
|
60.0
|
98.67
|
Protruding incisor
|
4.6
|
95.9
|
2.5
|
97.79
|
Mallampati scoring system
|
77.3
|
98.2
|
48.57
|
99.5
|
Cormack and Lehane’s scoring system
|
100
|
99.7
|
88
|
100
|
Discussion
Difficulty in endotracheal intubation constitutes an important
cause of morbidity and mortality, especially when it is not anticipated
preoperatively. This unexpected difficulty in intubation is the result
of a lack of accurate predictive tests and inadequate preoperative
assessment of the airway. Risk factors if identified at the preoperative
visit help to alert the anaesthetist so that alternative methods of
securing the airway can be used or additional expertise sought before
hand.
Direct laryngoscopy is the gold standard for tracheal intubation.
There is no single definition of difficult intubation but the ASA
defines it as occurring when “tracheal intubation requires multiple
attempts, in the presence or absence of tracheal pathology”. Difficult
glottic view on direct laryngoscopy is the most common cause of
difficult intubation. The incidence of difficult intubation in this
study is similar to that found in others.
As for as the predictors are concerned, different parameters for
the prediction of difficult airways have been studied. Restriction of
head and neck movement and decreased mandibular space have been
identified as important predictors in other studies. Mallampati
classification has been reported to be a good predictor by many but
found to be of limited value by others14. Interincisor
gap, forward movement of jaw and thyromental distance have produced
variable results in predicting difficult airways in previous studies7,15. Even though thyromental distance is a measure of mandibular space, it is influenced by degree of head extension.
There have been attempts to create various scores in the past. Many
of them could not be reproduced by others or were shown to be of
limited practical value. Complicated mathematical models based on
clinical and/or radiological parameters have been proposed in the past16,
but these are difficult to understand and follow in clinical settings.
Many of these studies consider all the parameters to be of equal
importance.
Instead of trying to find ‘ideal’ predictor(s), scores or models,
we simply arranged them in an order based on the strength of association
with difficult intubation. Restricted extension of head, decreased
thyromental distance and poor Mallampati class are significantly
associated with difficult intubation.
In other words patients with decreased head extension are at much
higher risk of having a difficult intubation compared to those with
abnormalities in other parameters. The type of equipment needed can be
chosen according to the parameter which is abnormal. For example in a
patient with decreased mandibular space, it may be prudent to choose
devices which do not involve displacement of the tongue like the Bullard
laryngoscope or Fiber-optic laryngoscope. Similarly in patients with
decreased head extension devices like the McCoy Larngoscope are likely
to be more successful.
Conclusion
This prospective study assessed the efficacy of various parameters of airway assessment as predictors of difficult intubation. We have find that head and neck movements, high arched palate, thyromental distance & Modified Malampatti classification are the best predictors of difficult intubation.
This prospective study assessed the efficacy of various parameters of airway assessment as predictors of difficult intubation. We have find that head and neck movements, high arched palate, thyromental distance & Modified Malampatti classification are the best predictors of difficult intubation.
| Competing Interests None Declared Author Details ARUN KUMAR GUPTA, Dept. Of Anaesthesiology, Rural Medical College, Loni, MOHAMED OMMID, Dept. Of Anaesthesiology, SKIMS, Soura, J&K, India SHOWKAT NENGROO, Dept. Of Anaesthesiology, SKIMS, Soura, J&K,India IMTIYAZ NAQASH, Dept. Of Anaesthesiology, SKIMS, Soura, J&K,India ANJALI MEHTA, Dept. Of Anaesthesiology, GMC Jammu, J&K, India CORRESSPONDENCE: ARUN KUMAR GUPTA, Assistant Professor Dept. of Anaesthesiology & Critical Care Rural Medical College, Loni Maharashtra, India, 413736 Email: guptaarun71@yahoo.com |
References
1. Rose DK, Cohen MM. The airway: problems and predictions in 18,500 patients. Can J Anaesth 1994; 41:372-83.
2. Benumof JL: Management of the
difficult airway: With special emphasis on awake tracheal intubation.
Anesthesiology 1991; 75: 1087-1110
3. Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Predicting difficult intubation. Br J Anaesth 1988; 61(2):211-6.
4. A.Vasudevan, A.S.Badhe. Predictors of difficult intubation – a simple approach. The Internet Journal of Anesthesiology 2009; 20(2)
5. Tse JC, Rimm EB, Hussain A. Predicting
difficult endotracheal intubation in surgical patients scheduled for
general anesthesia: a prospective blind study. Anesth Analg 1995; 81(2):254-8.
6. Savva D. Prediction of difficult tracheal intubation. Br J Anaesth 1994; 73(2):149-53.
7. Butler PJ, Dhara SS. Prediction of
difficult laryngoscopy: an assessment of the thyromental distance and
Mallampati predictive tests. Anaesth Intensive Care 1992; 20(2):139-42.
8. Mallampati SR, Gatt SP, Gugino LD,
Desai SP, Waraksa B, Freiberger D, et al. A clinical sign to predict
difficult tracheal intubation: a prospective study. Can Anaesth Soc J 1985; 32(4):429-34.
9. Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia 1987; 42(5):487-90.
10. Nath G, Sekar M. Predicting difficult intubation--a comprehensive scoring system. Anaesth Intensive Care 1997; 25(5):482-6.
11. Charters P. Analysis of mathematical model for osseous factors in difficult intubation. Can J Anaesth 1994; 41(7):594-602.
12. Arne J, Descoins P, Fusciardi J, Ingrand P,
Ferrier B, Boudigues D, et al. Preoperative assessment for difficult
intubation in general and ENT surgery: predictive value of a clinical
multivariate risk index. Br J Anaesth 1998; 80(2):140-6.
13. Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984; 39(11):1105-11.
14. Lee A, Fan LT, Gin T, Karmakar MK, Ngan Kee WD. A
systematic review (meta-analysis) of the accuracy of the Mallampati
tests to predict the difficult airway. Anesth Analg 2006; 102(6):1867-78.
15. Bilgin H, Ozyurt G. Screening tests for predicting difficult intubation. A clinical assessment in Turkish patients. Anaesth Intensive Care 1998; 26(4):382-6.
16. Naguib M, Malabarey T, AlSatli RA, Al Damegh S,
Samarkandi AH. Predictive models for difficult laryngoscopy and
intubation. A clinical, radiologic and three-dimensional computer
imaging study. Can J Anaesth 1999; 46(8):748-59.
Tidak ada komentar:
Posting Komentar